What We Can Learn From a Tiny Baltic Country’s Two-Decade Fentanyl Crisis
January 6, 2020Every summer, Estonia’s medieval capital Tallinn—a ferry ride from Finland and a day’s drive from Russia—buzzes with American and European tourists. They disembark from cruise ships docked on the glassy Baltic sea or arrive on budget air flights to visit Tallinn’s cobbled streets, bars, and relics of the country’s resented Soviet occupation.
An EU and NATO member since 2004, Estonia now looks to Scandinavia and wider Europe for inspiration. The country has linguistic similarities with Finnish, a flourishing "new Nordic" cuisine scene, and has become one of the most digitized nations on earth.
But Estonia’s bright new era masks a hidden problem the tourists rarely encounter, a legacy of the split from Soviet rule in 1991. For almost two decades, Estonia and its legion of Russian-speaking addicted opioid users, have been battling the world’s longest documented fentanyl epidemic. The country, which has just 1.3 million people – the population of Dallas, Texas – is the only zone outside of North America to have suffered so severely from the introduction of the synthetic opioid into its heroin food chain.
So how did fentanyl come to dominate heroin in this small country in Europe’s north eastern corner? And crucially, what lessons for its own spiralling opioid crisis can North America learn from Estonia’s protracted experience?
On a rainy day in an unloved part of Tallinn last August I met Sasha*, a long-term opioid user in his 40s. Sasha had several front teeth missing, and his arms bore stick-and-poke tattoos—one of a blissfully serene woman—and also deep track marks.
Even though fentanyl has a more powerful initial high than heroin, it’s shorter lasting. So for Sasha, fentanyl was an expensive habit, especially as his tolerance grew quickly. “I had to steal a lot, because the dose increases very quickly, and this much money cannot be found anywhere,” he said. At one point it took 200 Euros a day of fentanyl just to feel normal. "In the morning you wake up, you need to go and get large amounts of money. This leads to jail. I also lost my family because of this. [The drug] did not lead to anything good. My whole circle of friends is the same drug addicts, former drug addicts, people who steal, and so on. I must have a blue passport. I don’t have it …I have to have a place to live. I don’t have it either.”
Years of drug abuse resulted in Sasha spending several stints in jail, the death of scores of his friends, estrangement from his family and a life in poverty and debt. Sasha is one of Estonia’s “grey passport” holders, people of Russian descent who never took Russian or Estonian citizenship after the collapse of the Soviet Union in 1991 and who remain essentially stateless while living in the EU. He is one of around 15,000 to 20,000 injecting drug users in Estonia, the majority of whom are Russian-speakers based in the country’s north and east.
“I would say right now, two out of ten people are Estonian-speaking and eight out of ten, Russian,” said Greete Org, a project manager who works at a harm-reduction service in the capital and is a former amphetamine injector whose own friends injected opioids. “Someone really, really close to me died by overdosing on fentanyl,” she recalled. “I didn’t see her dying, but I woke up and she was dead. I contacted emergency services and they came, they couldn’t do anything,” she said. “They said ‘don’t cry, she’s a junkie, and junkies always die’, and that was something that changed me. I didn’t want to be just a junkie. I didn’t want to be just an overdose statistic.”
Half of all injecting drug users in Estonia have HIV. Many of these started on the route to addiction after the reintroduction of the native Baltic languages in Estonia meant that local Russian-speakers lost jobs and found it harder to gain employment.
Estonia’s proportionally large number of addicted opioid users turned onto fentanyl after a series of events 2,500 miles away in Afghanistan, just after the turn of the millennium.
In July 2000, the Taliban ordered a year-long ban on opium poppy cultivation in Afghanistan, a country that produces 90 percent of the world’s illicit heroin supply. The ban, a doomed effort by Taliban leaders to improve their image on the international stage, triggered a shortage of heroin in many parts of the world in the early 2000s.
In the more lucrative Western European markets and Russia, the shortage was less pronounced, although users had to put up with a more diluted product. In Pakistan and India, where the drought hit hard, heroin users instead used black market buprenorphine, an opioid used to treat heroin addiction. The same drug replaced heroin in Finland. But in Estonia, whose population of heroin users were left high and dry by the Taliban’s poppy ban, it was the potent opioid fentanyl that filled the gap.
Why the heroin shortage led to Estonia adopting fentanyl is not completely clear, although the country’s connections with Russia and its relatively high number of heroin users appear to be key factors.
Supply was close at hand. Estonia is just 99 miles from St Petersburg, Russia’s northern capital, where fentanyl labs were detected in the 1990s. Similar drug labs were later found in Estonia, near the Russian border. Producing and distributing fentanyl, marketed to users as “china white,” became an easy and lucrative piece of business for Russian-speaking Estonian organized crime groups, who were already linked in to Estonia’s large Russian-speaking population of drug users.
From 2003 onwards, fentanyl use snowballed and so did fatal drug overdoses and new cases of HIV. By 2012, this small country had one of the highest overdose death rates in the world. In 2017, Estonians were six times more likely than the average European to die from a drug overdose. Because of fentanyl’s shorter-acting nature, opioid users started injecting more frequently every day, increasing the risk of spreading blood-borne infections such as HIV. In 2003 there were 1,500 new HIV cases, a record high.
This galvanized the government. From 2004, assisted by public health money from the Global Fund, harm-reduction services such as methadone treatment, cognitive behavioral therapy and needle exchanges were introduced. New HIV cases started to fall and so did the number of deaths, partly because of the distribution, starting in 2013, of take-home naloxone, the drug used to reverse opioid ODs.
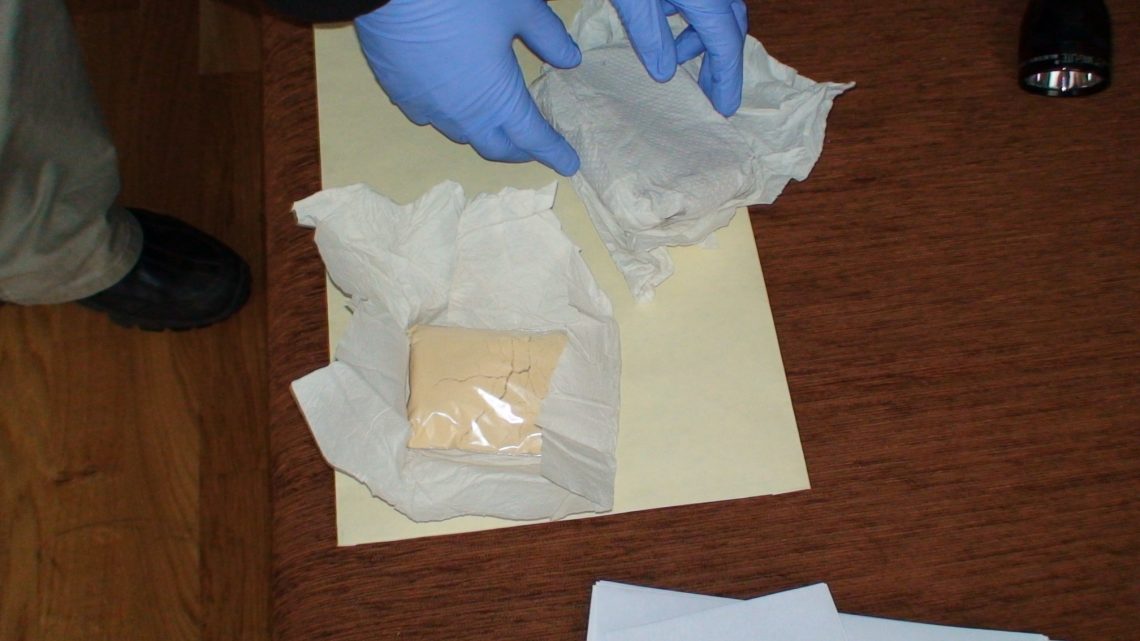
Then the police finally caught up with the fentanyl barons. In May 2017, a massive police operation took out 10 to 15 key individuals from the country’s main fentanyl distribution networks. The networks responsible, from street dealers using dead letter boxes and forest caches to people at the top dealing hundreds of grams, were operating primarily around Tallinn in the north and to a lesser extent in Ida-Viru County, in the country’s east, where Estonia shares a border with Russia.
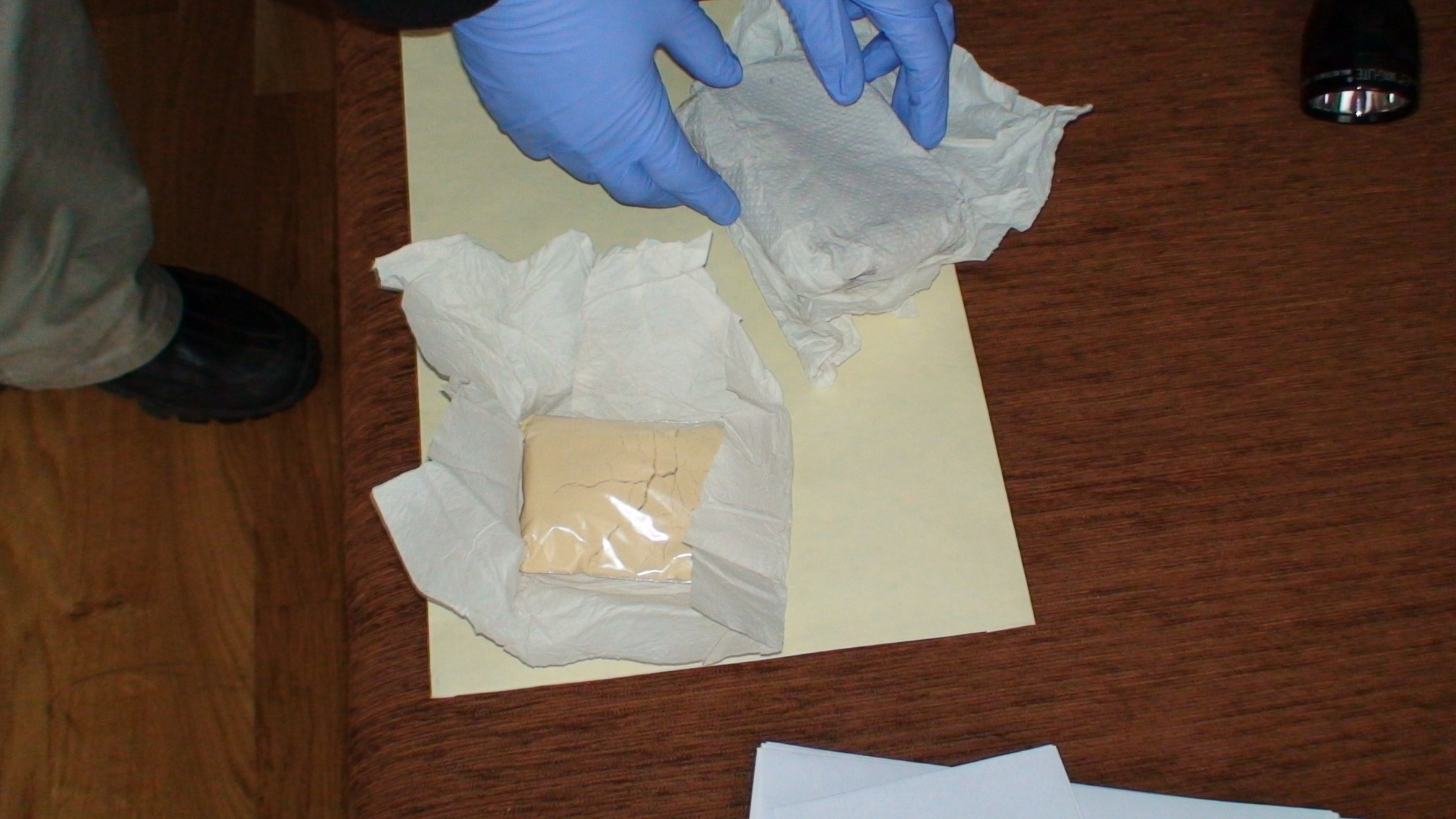
During 2017, 9.7kg of fentanyl – which at an average purity of 13 percent would have made around one million 1mg doses – was seized and several domestic laboratories taken down. The busts, which also unearthed 420g of two fentanyl analogues, furanyl fentanyl and super-potent carfentanil, successfully disrupted the domestic market in fentanyl and its analogues. It led to a severe shortage of the drug for six months and a fall in drug deaths to rates of 20 years ago, from a height of 170 in 2012 to 39 in 2018 and 24 in the first eight months of 2019.
The drought led users and suppliers to replace fentanyl with a variety of other trashy, injectable highs including amphetamines, black market prescription drugs, cathinones, even more potent fentanyl analogues such as carfentanil, cyclopropyl fentanyl and furanyl fentanyl and a synthetic opioid, isotonitazene.
At one syringe exchange point in the centre of Tallinn, a man named Vitya* was quivering erratically. Wearing a white baseball cap backwards, his dark hair escaped in thin wisps underneath, fading into his greying goatee. He told me he is a former fentanyl injector but now only injects amphetamines.
“I like amphetamines and I don’t want to stop,” he said. Vitya has seen fentanyl’s devastating effects firsthand. “Many of my friends died because of fentanyl. People who use drugs are always going to be junkies. It’s not a social problem, it’s a life.” Estonia’s harm-reduction centers help him by giving him something to eat and letting him shower and clean his things. He has friends who still use fentanyl, which he finds “sad, but I can’t do anything. I think we need heroin back because there will be fewer deaths.”
Even after the temporary crippling of fentanyl supply, heroin remains a highly elusive drug in Estonia. Sidelined by its more lethal cousins, it may have been banished for good and not just in the minds of drug suppliers. “There’s no point in using heroin anymore,” said Katri Abel-Ollo, from the Center for Addiction and Communicable Diseases Prevention at Estonia’s National Institute for Health Development. “They know heroin is safer and it’s easy to dose, but [compared to fentanyl and its analogues] it’s too weak, it’s like injecting water.”
Meanwhile since the crackdown on fentanyl, the drug trade has adapted and survived, as it almost always does. Fentanyl supply has been partially restored here , largely via the dark web, and often through neighbouring Latvia. Anneli Uusküla, a professor at the Department of Public Health at the University of Tartu, told VICE last month that fentanyl is still the main drug of injection in Estonia, with 70 percent of drug injectors using it in 2019.
So what lessons can North America learn from Estonia’s experience?
Jirka Taylor, a policy analyst at RAND who co-authored a deep dive report into the future of the global fentanyl trade, said although Estonia is a very small country, its experience needs to be considered as the U.S. and Canada attempt to navigate the biggest drug crisis they have faced.
“Estonia is the only window into how a market can look after nearly two decades of dominance of fentanyl and its analogues,” he told VICE. “What it shows is the staying power of fentanyl. Heroin has been successfully displaced and has not come back. There is now very little demand for heroin as users have become used to fentanyl.” He said that Estonia’s experience shows that while fentanyl increases deaths, it has not led to an increase in the number of users. He added that fentanyl appears to need an existing user population to take hold in a market.
Taylor described the “relative success” of Estonia’s police crackdown on fentanyl in 2017 as a “quite remarkable” event that could be transferred to North American cities or small states. “Perhaps there is scope for targeted innovative supply reduction efforts. Particularly for jurisdictions that may not have been affected by fentanyl as much yet and where there is great value in at least delaying its onset.”
Bryce Pardo, an associate policy researcher who co-authored the fentanyl report, said some parts of the U.S. have an“Estonia-like situation.” He said that in New Hampshire, for example, there are now very few heroin seizures or heroin-related overdose deaths because it’s dominated by fentanyl. “That is important, because as the market transitions to fentanyl, harms will increase and available policies and responses may not be enough” because of the heightened risk of overdose, transmission of bloodborne disease and increased crime, which, as happened in Estonia, “will have broad impacts on health and crime beyond overdoses and overdose emergency responses”.
For Professor Uusküla, who has spent many years documenting the plight of Estonia’s fentanyl users, the message for North America is that the best way of tackling the fentanyl crisis is to pool resources into harm reduction. “Based on experiences in Estonia, we would recommend large-scale implementation of evidence-based programmes in areas with high fentanyl use,” she wrote in a co-authored article published in the Lancet last month. This, the authors said, should include the “distribution of naloxone to reverse opioid overdoses; syringe service programmes to provide for safer injecting; opiate substitution treatment with minimal restrictions on patients so they might be integrated into community life; and community programmes to reduce initiation into injecting drug use.”
Ultimately, even if U.S. and Canadian enforcement agencies are able, city by city, to round up key fentanyl suppliers, fresh suppliers and even more insanely potent drugs will be waiting in the wings. But governments know all this. For decades now, prohibition has led to the spread of increasingly dangerous types of drugs, that are cheaper to make and less bulky to smuggle than the old ones.
As Estonia is still learning—and North America will learn too—the only way of stopping this deadly spiral is to do two things: Ensure harm-reduction measures are in place to help those at the highest risk of being killed by increasingly toxic substances, and to tackle the root causes of addiction, such as inequality and lack of hope, in order to slow the tide of people willing to take such huge risks in order to get through the day.